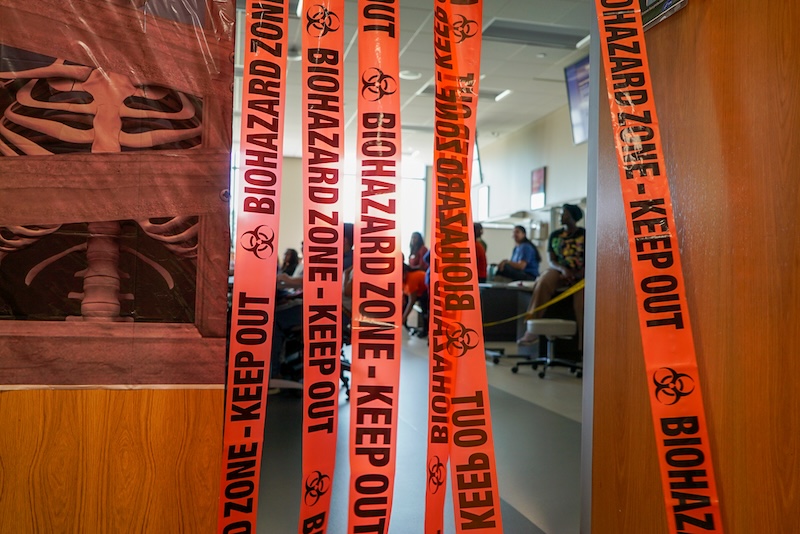
Campbell healthcare students walked beyond the caution tape, into dark rooms, where ghosts hovered and witches lurked. Unmistakably Halloween.
On Oct. 15, Smith Hall became the “Haunted Hospital in the Creek.”
Tricks and treats aside, in this haunted hospital learning was key.
Students in the College of Pharmacy and Health Sciences and the Jerry M. Wallace School of Osteopathic Medicine participated in one of the University’s Interprofessional Case Study learning activities, which are offered several times a year, said Dr. Pamela Edwards, assistant dean for Interprofessional Education and chair and director, Catherine W. Wood School of Nursing.
Representing the Nursing, Physician Assistant, Public Health, Pharmacy, Osteopathic Medicine and Physical Therapy programs, students split into groups and throughout the day traversed six learning stations, including, for example, a “Ghostbusters” event and “Mad Scientist” room.
Each group of students represented a mixture of the healthcare disciplines.
The students created case studies and designed unique health-related contributions, all in the Halloween spirit. Each healthcare discipline decorated a room, and some students, faculty and staff showed up in costume.
Jamie Hart, a Physician Assistant and assistant professor, led the “Ghostbusters” session, which focused on dispelling myths about PAs. Students responded to a group of questions, such as, Can PAs assist in surgeries? They can. Can they prescribe medication in all 50 states? Yes. They treat patients of all ages? Correct.
“Everyone got them all right,” Hart said.
Hart talked about recent state legislation that included joining the Physician Assistant Interstate Licensure Compact and reducing some supervisory requirements for PAs.
“A PA that graduated a year ago is probably different than a PA that graduated 20 years ago, in their abilities and that kind of thing,” Hart said.
The “Mad Scientist” session provided lessons on osteopathic medicine, in this case focusing on a patient with severe chemical burns.
Krystle Edge, assistant director of Nursing and an assistant professor, led a group of students who assessed the patient and decided on treatment options. The students first scoured for clues, placed throughout the room, to guide them through care.
Students worked on estimating what percentage of the body was burned. Severe burns lead to swelling and other complications, sending the body into a type of shock. The healthcare professors estimate the burn percentage and use a formula to determine how much fluid to give the patient to maintain, for example, blood pressure and perfusion to organs. The students also learned about giving patients the correct and incorrect medications to relieve pain.
“One of the big things about burns is the risk for infection,” Edge says. Which involves properly treating and bandaging the wound.
The biggest danger to a burn patient within the first 24 hours is shock caused by fluid shifts. Beyond that is the risk of infection.
“We hit both of those,” Edge said.